A hysteroscopy is a procedure doctors use to diagnose and treat conditions involving the uterus and cervix, such as abnormal uterine bleeding, abnormal endometrial thickening, bleeding after menopause, and infertility.
During a hysteroscopy, your doctor inserts a hysteroscope – a thin tube with a light on the end – into your vagina, through your cervix, and into your uterus. They’ll be able to see into your cervix and inside your uterus. They can take a sample for later testing if they find anything abnormal.
Diagnostic Hysteroscopy
A diagnostic hysteroscopy allows a doctor to check for causes of abnormal uterine bleeding. Doctors may use a this procedure to diagnose conditions including:
- Abnormal endometrial thickening.
- Postmenopausal bleeding.
- Blocked fallopian tubes.
- Endometrial cancer.
- Intrauterine adhesions (IUAs), or scar tissue in the uterus.
- Infertility.
Operative Hysteroscopy
An operative hysteroscopy is surgery that puts a hysteroscope through the cervix into the uterus. It’s used to treat abnormalities in the uterus. A doctor may recommend an operative hysteroscopy for conditions like:
- Abnormal uterine bleeding.
- Fibroids.
- Other disorders of the uterus.
A doctor may use an operative hysteroscopy for surgeries to treat conditions affecting the vagina, cervix, and uterus. These surgeries include:
- Endometrial ablation, to destroy the uterine lining.
- Septum resection, to treat a vaginal septum, or wall of tissue dividing the vagina.
- Myomectomy, to remove fibroids without removing the uterus.
- Polypectomy, to remove any abnormal growth in the uterus.
A doctor may do a diagnostic and operative hysteroscopy in the same procedure so that you won’t have to have another surgery to treat any issue they found.
Why would You need a Hysteroscopy?
The most common reasons for a hysteroscopy are periods that are longer or heavier than normal or bleeding between periods. You might need the procedure in these situations:
- Your Pap test results are abnormal.
- You’ve been bleeding after menopause.
- There are fibroids, polyps, adhesions, or scarring on your uterus.
- You’ve had more than one miscarriage.
- You've had problems with infertility.
- Your doctor needs a small tissue sample (biopsy) of the lining of your uterus. You might have a hysteroscopy with a biopsy before you get a dilation and curettage (D&C) procedure to remove more tissue from the uterine lining.
- Your IUD has come out of place.
- To confirm the results of an ultrasound, hysterosalpingography (HSG), or other tests looking at the cervix and uterus.
- To open blocked fallopian tubes.
- To place birth control implants that close off the fallopian tubes.
- For surgery to treat fibroids, polyps, scarring, and more.
- Together with a laparoscopy, which allows your doctor to see the outside of your uterus as well as other organs in your pelvis.
- At times, a hysteroscopy might be done along with an endometrial biopsy before a full D&C procedure.
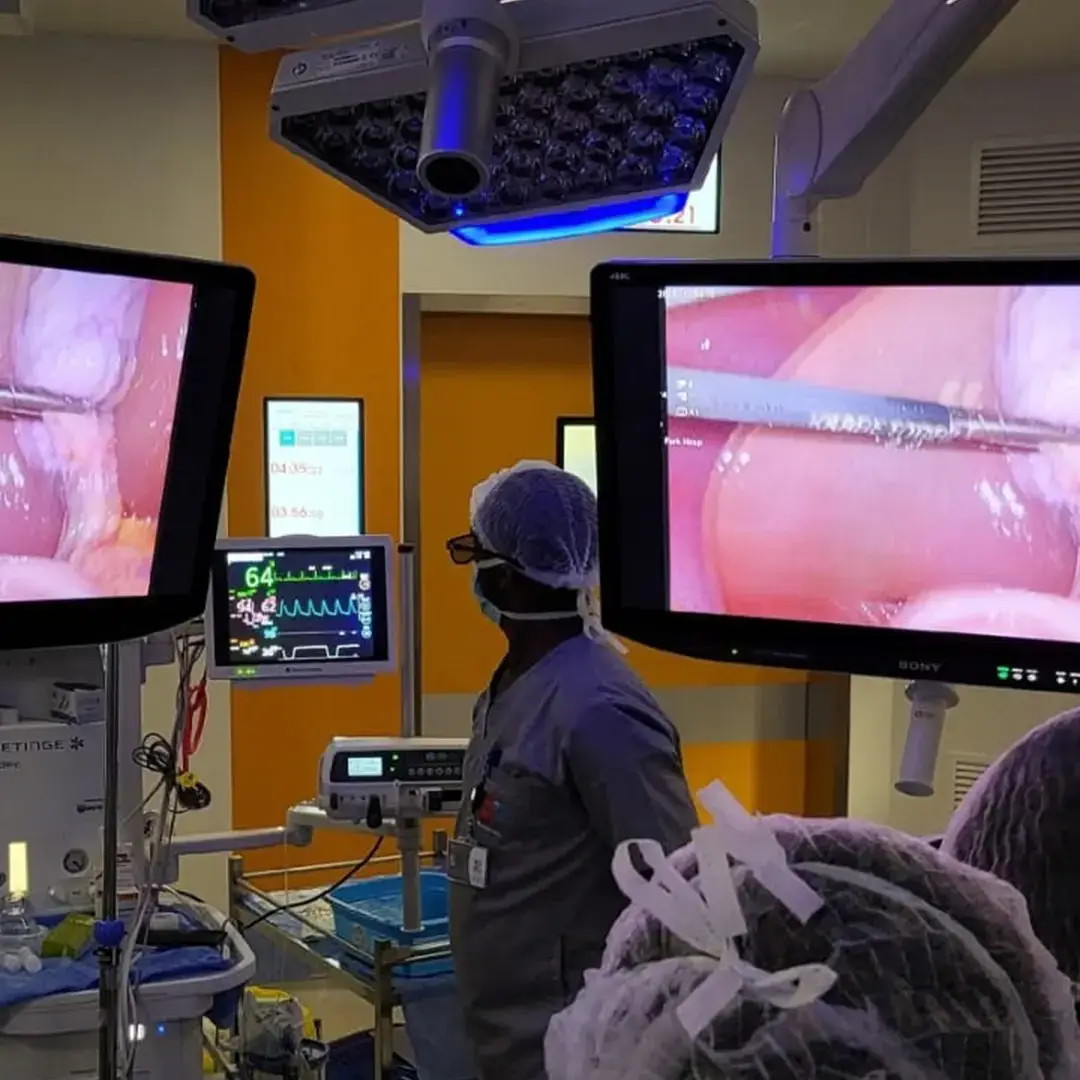
Hysteroscopy Procedure
You can have a hysteroscopy in a hospital or at your doctor’s office. During the procedure, you may be awake under local or regional anesthesia or asleep under general anesthesia. If you’re having general anesthesia, your doctor may ask you not to eat or drink anything for 6 to 12 hours. If you’re awake, your doctor will give you medicine to help you relax. They’ll also use medication or tools called dilators to help open your cervix.
Your doctor will likely use a tool called a speculum to keep your vagina open. If you’ve ever had a Pap test, your doctor probably used one during that procedure, too.
They’ll gently insert the hysteroscope through the cervix into your uterus and push gas or a liquid-like saline through the hysteroscope into your uterus to expand it. This will give them a clear view of its lining and the opening of your fallopian tubes.
They’ll then see the insides of your uterus with the images that appear on a video monitor.
If the hysteroscopy is to treat conditions like polyps or fibroids, your doctor will insert the devices for removing the abnormal tissue through the hysteroscope.
The best time to do a hysteroscopy if you have regular periods is the first week after your period ends. You may have a hysteroscopy at any time if you’re past menopause. A doctor will not do a hysteroscopy if you:
- Are on your period.
- Are pregnant.
- Have a pelvic infection.
- Have genital herpes or signs that you might have it.
- Have cervical or endometrial cancer.
A doctor might also not recommend a hysteroscopy if you have heart disease or tend to bleed easily. Speak with your doctor about any health conditions you might have before a hysteroscopy.
Tell your doctor if you unexpectedly get your period on the week of the procedure. They may need to reschedule it. Also, don’t use vaginal medicines, a douche, or a tampon 24 hours before your procedure.
Patients' Testimonials
Need to book an appointment?
Other Gynaecology Services